- The 2023-2024 California state budget guaranteed that funds raised from the individual mandate tax penalty will be used to lower costs for Californians who purchase care on their own through Covered California.
- Covered California’s Board voted today to use the funds to implement new 2024 benefits that will significantly reduce deductibles and co-pays for over 650,000 Californians.
- This act zeroes-out hospital deductibles in Silver plans for those under 250% of the poverty level—deductibles that would have been as much as $5,400.
- These lower costs will ensure that more Californians will be able to purchase and access the care they need to get and stay healthy.
SACRAMENTO, CA–While usually not set to meet in July, Covered California held a board meeting today to vote to ensure that funds authorized from the recently signed state budget are used to significantly reduce co-pays and deductibles in many 2024 health plans. As a result, over 650,000 Californians will have more access and affordability to health care, from doctor visits to prescription drugs to hospital stays. A family of four with an income of $69,000 a year would have their hospital deductibles eliminated—which otherwise might have been as much as $5,400.
Earlier this month, Governor Newsom signed the 2023-2024 state budget which authorized the funds to go to lower out-of-pocket costs for many Covered California enrollees. A top priority for health care advocates and several state legislators including Assemblywoman Pilar Schiavo, author of related AB 1208¬, this budget victory means that most of the money raised from the tax penalty on those without health insurance is now reserved specifically to lower costs for health care.
The 2023-2024 state budget allocates $82.5 million to the Health Care Affordability and Reserve Fund to lower costs for Covered California enrollees in 2024, and $165 million in 2025 and beyond. Using the $82.5 million investment, today Covered California’s board approved a new benefit design for over 650,000 Silver plan enrollees in the 2024 plan year. Such benefits include lower or zeroed-out deductibles and reduced co-pays. Another 35,000 will be automatically enrolled into these higher-value plans to receive the new benefits.
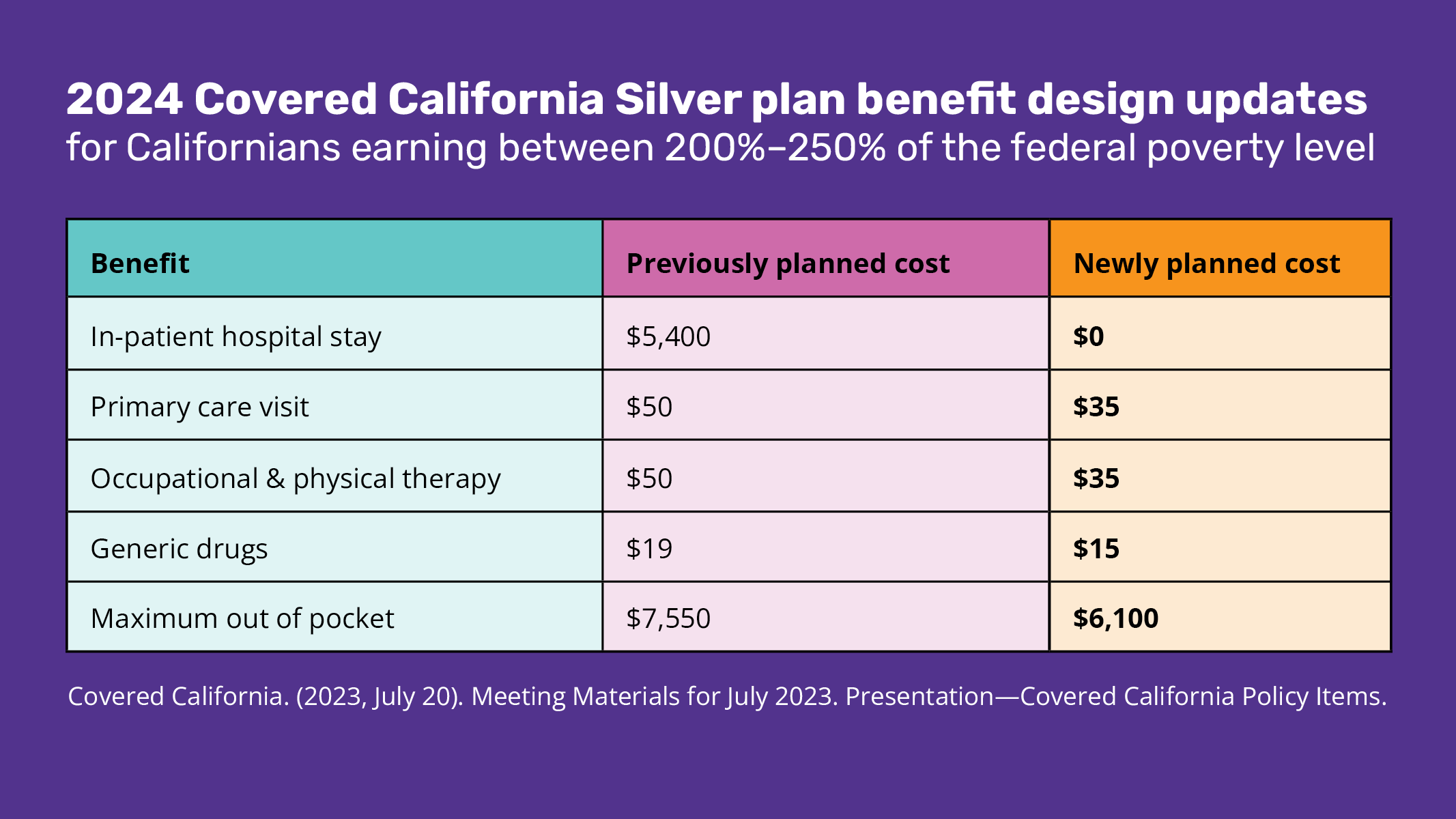
The majority of Covered California enrollees earn between 138% and 250% of the federal poverty level and will be the population most directly affected by these new benefit designs. The table below shows how the new 2024 benefits will impact Californians earning between 200% and 250% of the federal poverty level ($27,180/year – $33,975/year for an individual; $55,500/year – $69,375/year for a family of 4):
“This is huge–hundreds of thousands of Californians will be able to better access and afford hospital stays, doctor visits, prescription drugs, and more. Many low-income Californians were going to see their hospital deductibles rise to nearly $5,500, and now those will be eliminated,” said Diana Douglas, Policy and Legislative Director for Health Access California. “These new benefits will provide real relief to many in Covered California plans who are struggling to afford their health care costs. This action means more Californians will be able to access care and not be hit with a huge bill.”
These lower costs also come at a critical time when many people may soon be determined ineligible for Medi-Cal after a pause in redetermination during the pandemic. Those that may be losing Medi-Cal and looking to purchase coverage through Covered California will now be eligible to receive these enhanced benefits and are more likely to get and remain covered.
These benefits are only for 2024 coverage. New benefits will be established upon the larger allocation of funds for this purpose in 2025.
“We are excited that Covered California is reducing cost-sharing this year with more planned for next year, to lower these financial barriers to care that harm those that need help most often. It is great that California is seeking to eliminate deductibles that have climbed to over $5,000, putting patients in financial distress at the same time as they are experiencing medical crises,” said Anthony Wright, Executive Director, Health Access California. “This action is a great example of how policymakers, patient advocates, legislators and the Governor can come together to provide real relief for affordability and keep a promise to use health care dollars for health care.”
###