In a medical emergency, you may be thinking a lot of things – am I ok? Do I need help? Can I get to a hospital? The things you should not be thinking are “can I afford the ambulance ride I need?” or “is this ambulance provider in my network?”
Yet many Californians have received a surprise bill after taking an ambulance. A surprise bill happens when a person is unknowingly seen by an out-of-network provider for a service. In the case of ambulances, the consumer has no choice whether the ambulance that arrives is contracted with their health plan, resulting in large surprise bills.
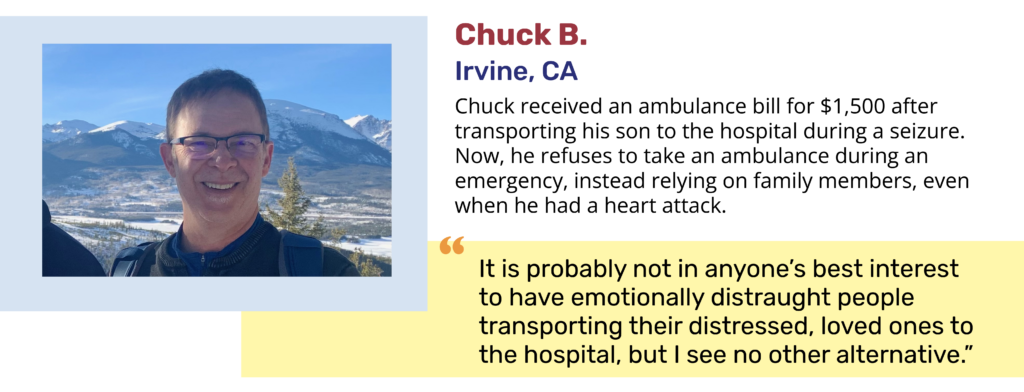
Chuck is one of the Californians who has faced an unexpected and expensive bill after an ambulance ride. Now, he won’t call 911 because he fears the high cost. This shouldn’t happen to anyone who experiences a medical emergency.
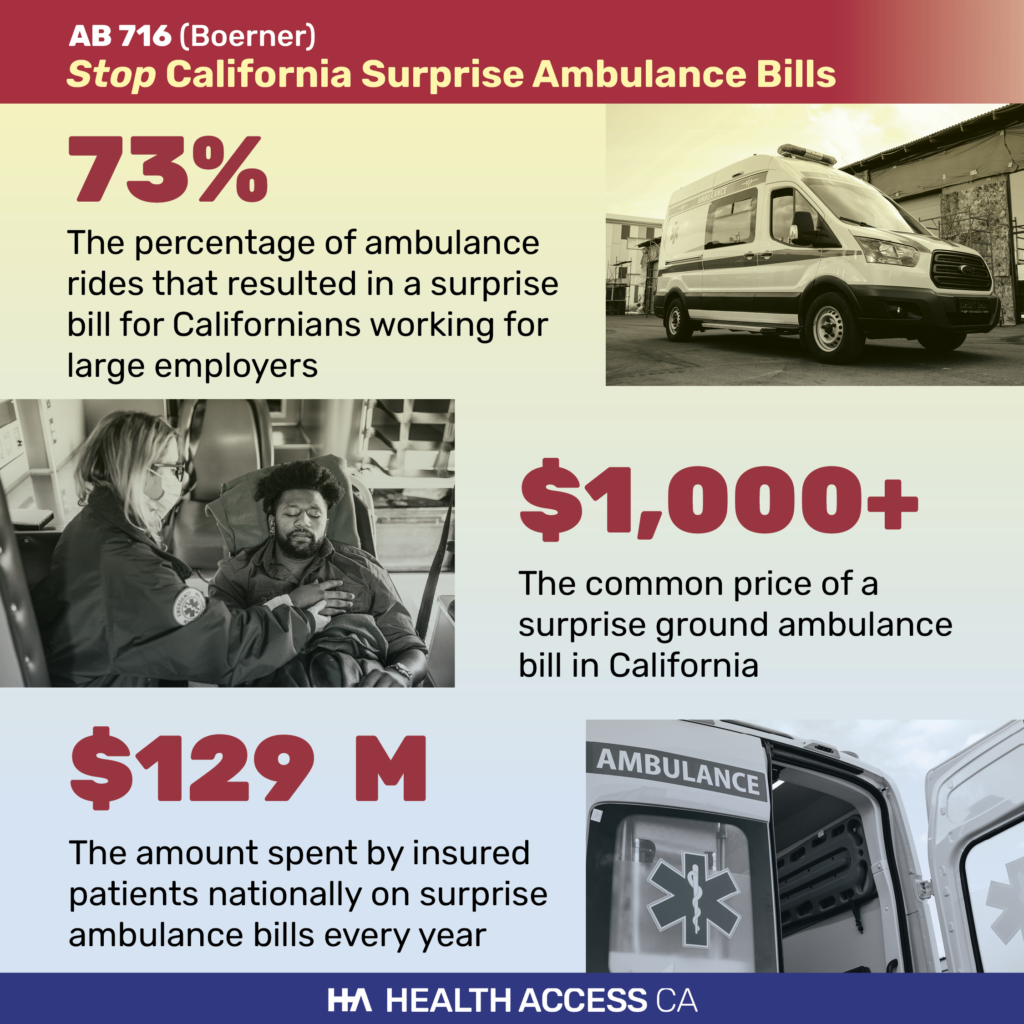
California is one of three states where a surprise ambulance bill costs over $1,000, and they can cost more than $2,000 depending on insurance providers. This can be financially destabilizing, especially for low- and moderate-income Californians who lack significant savings.
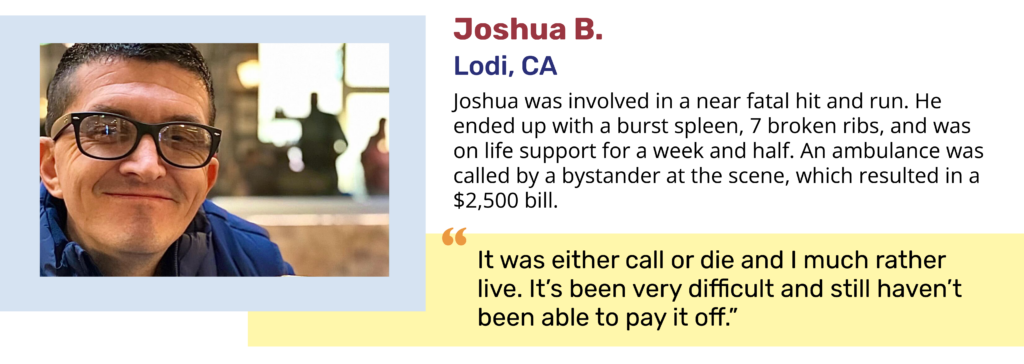
In many cases, a person in an emergency does not call an ambulance themselves or is unable to request an in-network provider at the time of the 911 call. Californians like Joshua (below) receive ambulance rides at the goodwill of a bystander. Only some weeks after they are out of the hospital do they face the cost of their life-saving care.
California has led the way to stop surprise medical bills, but ambulances remain a gap in current law. This year the California State Legislature has the opportunity to stop these bills this by passing AB 716 by Assemblymember Tasha Boerner.
Because it’s the right thing to do, the bill has already received bi-partisan support in two committees. Jennifer (below), yet another Californian impacted by surprise ambulance bills, shared her story in hearings at the California State Capitol.
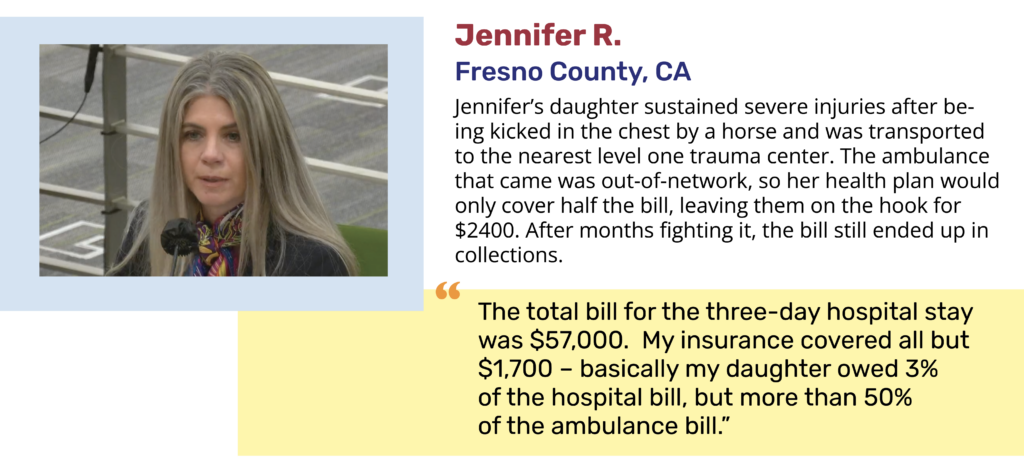
AB 716 gives Californians the peace of mind to know that calling 911 in an emergency will not mean being hit with a surprise bill that could destabilize their finances. The bill also ensures that there are protections in place to give consumers time to pay their bill, so that they aren’t sent to collections, like Jennifer and many others were.
With AB 716, Californians will have more financial security during and after a medical emergency and will be less hesitant to call 911 out of fear of a large surprise bill.
Want to support our work and help get this bill across the legislative finish line?


